- Industries
Industries
- Functions
Functions
- Insights
Insights
- Careers
Careers
- About Us
- Healthcare
- By Omega Team

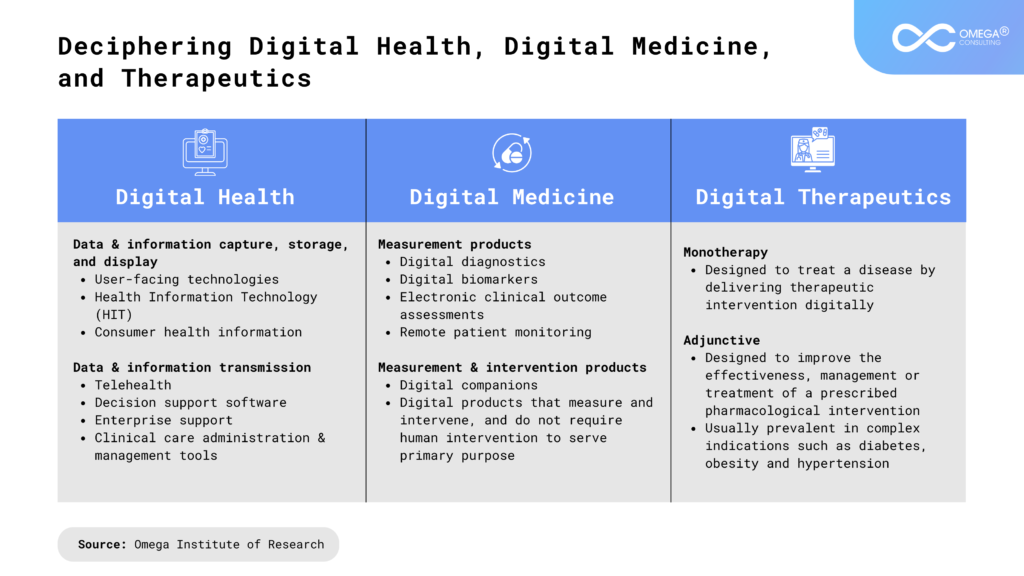
Digital therapeutics, a subset of digital health, offers software-based interventions for diagnosing, managing, and preventing medical conditions. Backed by the Digital Therapeutic Alliance (DTA), these evidence-based therapies utilize high-quality software to complement or replace traditional treatments. They target chronic diseases like diabetes and mental health disorders, where behavioral changes are crucial for effective management. Recognized as a disruptive force in healthcare, digital therapeutics are poised to revolutionize patient care, aligning with the shift towards holistic health and personalized medicine. This transformative approach, driven by advancements in digital medicine, epigenetics, and artificial intelligence (AI), underscores the pivotal role of digital therapeutics in shaping the future of medicine.
History of Digital Therapeutics
In 1995, Boston medical doctor Dr. Joseph Kvedar introduced a program to teach students the technological aspects of delivering healthcare in non-traditional settings. He introduced the one-to-many healthcare model, which aimed to provide accessibility, convenience, and efficiency while reducing workload and increasing physician scope. This model was considered one of the pioneers in digital health and DTx. The term “e-patient” was first used by Dr. Tom Ferguson in 1999, but it gained prominence ten years later. Since 2012, the term “DTx” has been used formally.
- Patients “equipped, enabled, empowered, and engaged in their health and health care decisions” are called “e-patients.”
- Many patients are becoming healthcare advocates, using tools to make informed decisions.
- The community’s heroes are the guests, who call doctors for tech medicine concerns.
- The contribution of digital health care and technology to a society prioritizing education is significant.
Key Drivers of Adoption
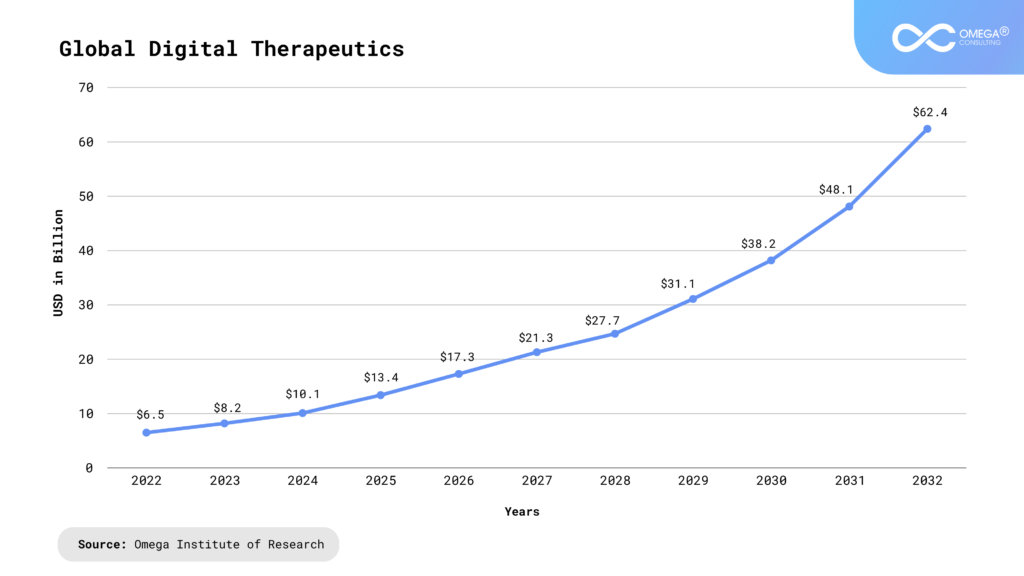
More investments in digital therapeutics are taking place now, considering the growing medical process and the need for less healthcare money. This industry is projected to grow at 19.83%, accounting for USD 9.65 billion between 2020 to 2028. There should be an increase of 1.67% for 2024 user penetration, which is set to reach 3.44% by 2028.
Digital Therapy in Mental Health Treatment
- Accessibility: Digital therapy breaks barriers for those in remote areas, with disabilities, or busy schedules.
- Convenience: It allows therapy from home, offering flexibility and eliminating travel time.
- Anonymity and Privacy: Online platforms offer confidentiality, easing concerns about stigma or judgment.
- Cost-Effectiveness: It’s often cheaper for both therapists and clients due to lower overhead and reduced travel expenses.
- Evidence-Based Interventions: Many platforms provide scientifically-backed treatments like CBT and DBT.
- Continuous Support: Some offer messaging for ongoing assistance between sessions.
- Customization and Personalization: Algorithms tailor treatment plans to individual needs, enhancing outcomes.
Digital Therapeutics: Versatile Alternatives
- Provides alternatives to conventional medical treatments.
- Can be used alone or with other therapies or pharmaceuticals.
- Future treatment options should cover broader medical, psychological, and behavioral issues.
Benefits of digital therapeutics for every stakeholder

Obstacles to Digital Therapeutics (DTx) Adoption
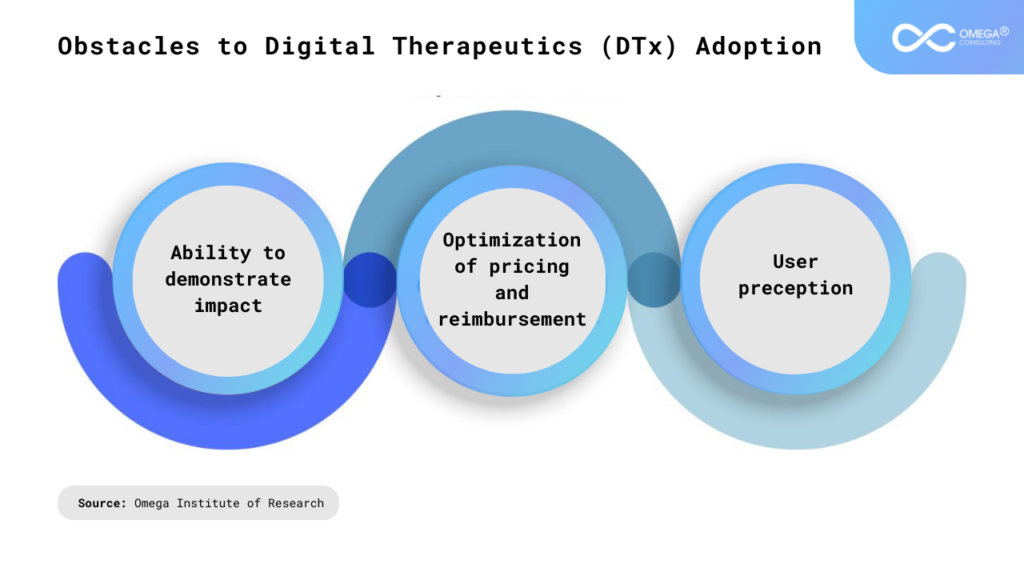
Ability to demonstrate impact
High-level trials and real-world results that can prove the effectiveness of digital medicines need to be displayed to shed some light on their benefits. The financial as well as medical implications must be shown. Manufacturers may need to go through RCTs page after page in reputable magazines, which will help prove that there are measurable outcomes. Prescriber support and adoption of digital therapies can also be done without solid proof; evidence-based studies were and still are the hub of everything [10].
Optimization of pricing and reimbursement
Regulatory uncertainty is a significant hurdle digital therapeutics encounter worldwide regarding reimbursement and coverage. While such solutions encounter some problems, the detailed real-world data about them can become an advantage in trying new types of contracts, outcomes-based or pay-for-performance ones, especially in countries like Germany.
User Perception
Adopting digital therapeutics on the patient’s side faces obstacles such as an unexplained decline in the patient’s initial eagerness to engage. Socioeconomic inequality may contribute to the aggravation of health inequalities about using PPEs. The privacy issues, particularly the real-time monitoring, raise questions. HCPs, as a rule, adopt DTx only slowly, and this hesitance restrains the notion of the payers. Implementation difficulties, including workflow adjustment and educational programs for staff, could jeopardize healthcare capacities. Overcoming these obstacles is essential for achieving the target of digital therapeutics, that is, to improve patient outcomes and medical efficiency [11].
Deciphering Digital health, digital medicine & digital therapeutics
SWOT Analysis
SWOT analysis is a strategic planning tool used to evaluate the Strengths, Weaknesses, Opportunities, and Threats of a business, project, or decision. Here’s a brief overview:
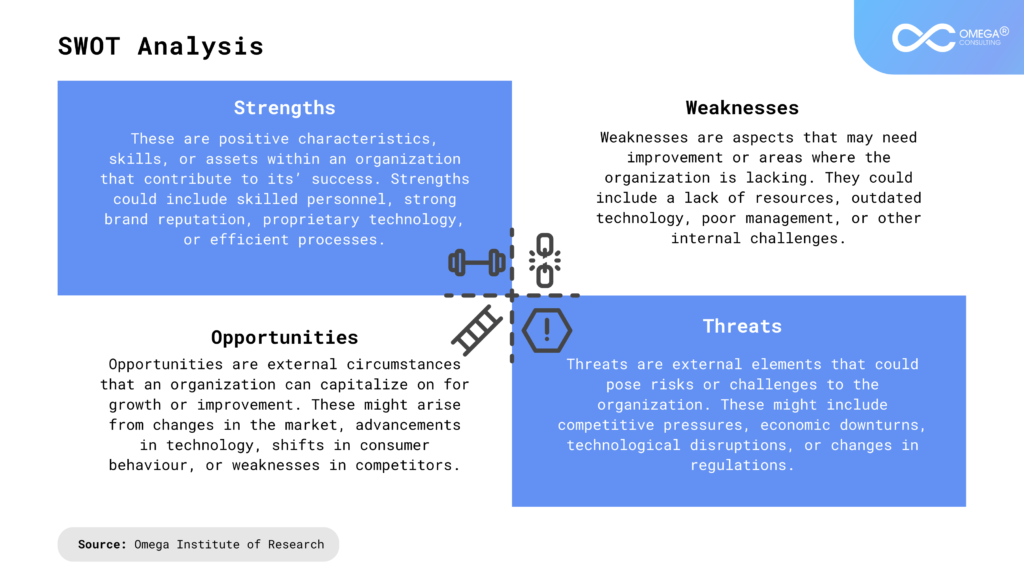
Strengths
By utilizing cutting-edge technology like artificial intelligence (AI) and data analytics, digital therapies provide scalable, customized healthcare solutions. They improve accessibility and convenience by offering remote patient monitoring. Treatment effectiveness can be optimized by regularly updating these treatments based on real-time data. Furthermore, digital medicines frequently show cost-effectiveness compared to conventional therapies, which lowers healthcare costs.
Weaknesses
The crucial shortcoming is the appearance of a digital gap between groups of people who find it very hard to buy the necessary technology, let alone use it properly. Ethical issues and risks of unauthorized access are the main barriers in the data collection and transfer of sensitive health information from patient to patient, posing privacy and security concerns.
Opportunities
There are many prospects for cooperation between technology businesses and healthcare providers in the digital therapeutics sector. Ongoing technological improvements and growing acceptance of remote treatment create a favorable atmosphere. Regulatory bodies are changing to support digital therapies, creating market growth and reimbursement opportunities. Collaborations with pharmaceutical firms and integration with current healthcare systems may further increase the scope and effect of digital treatments.
Threats
The digital medicines business faces significant concerns due to regulatory uncertainty and the requirement for solid proof of safety and efficacy. The fast speed of technological progress necessitates ongoing adaptation in an environment of intense competition. Furthermore, a lack of confidence in the efficacy of digital therapies among patients and healthcare professionals may prevent their broad adoption. Cybersecurity risks and the possibility of data breaches may hamper the long-term success of digital therapeutics.
Use Cases
Behavioral Change & Guidance
Since 75% of US people struggle with sticking to their treatment plans, medication adherence is a real challenge for healthcare stakeholders. Hospital expenses related to noncompliance are estimated by the Pharmaceutical Research and Manufacturers of America (PhRMA) to be between $100 and USD 300 billion annually. The average expenditure of a hospital visit for a non-adherent patient is 3,575 dollars more than that of a fully adherent patient, stressing the influence of this problem in the financial world [12].
Medical Training & Patient Engagement
Virtual reality (VR) technology progresses and brings a bright future for care that will benefit physicians and patients. Increased investments and penetration of VR in medical treatment provide beneficial instruments for controlling chronic illnesses and developing tailored treatment plans. With the help of VR, trainees practice their skills. VR apps, the digital therapy tool, create imaginary worlds that help patients handle their anxiety in postoperative pain. According to the same study, patients who used VR headsets before surgery have had 73% pain relief and 80% less fear. These outcomes perfectly show the intention of virtual reality in medical settings [13].
Conclusion
As of now, Digital Therapeutics (DTx) stands at the forefront of healthcare innovation, poised for significant growth and adoption. With advancements in technology, increasing acceptance from healthcare providers, and regulatory support, DTx is proving to be a promising avenue for improving patient outcomes and reducing healthcare costs. However, challenges such as regulatory complexities, integration into existing healthcare systems, and ensuring data security and privacy still need to be addressed. Despite these hurdles, the current state of Digital Therapeutics presents a landscape brimming with potential, offering a new paradigm in healthcare delivery and patient management.
- https://wwwpewresearchorg/internet/2008/08/26/the-engaged-e- patient -population/ Published 2008 Aug 26; Cited 2020 Jan 09.
- https://wwwpewresearchorg/internet/2008/08/26/the engaged-e-patient-population/ Published 2008 Aug 26; Cited 2020 Jan 09.
- http://tsdr.uspto.gov/documentviewer?caseId=sn85765357&docId=FTK20121101070417#docIn dex=4&page= Cited 2020 Jan 09.
- https://www.statista.com/outlook/hmo/digital-health/digitaltreatment-care/digital-therapeutics/worldwide#revenue
- https://doi.org/10.1186/s13561-020-00273-0
- https://www.lark.com/blog/2018-4-12-thecost-ofmedication-nonadherence/#:~:text=An%20estimate%20from%20the%20Pharmaceutical,patient%20who%20h ad%20been%20compliant.
- https://www.stgeorges.nhs.uk/newsitem/vr-headsets-relaxing-patients-during-surgeryat-st georges/
Subscribe
Select topics and stay current with our latest insights
- Functions