- Industries
Industries
- Functions
Functions
- Insights
Insights
- Careers
Careers
- About Us
- Healthcare
- By Omega Team
Healthcare providers everywhere are being stretched to their limits. Some see artificial intelligence (AI) as a reprieve for the weary workforce, but it’s not without its limitations.
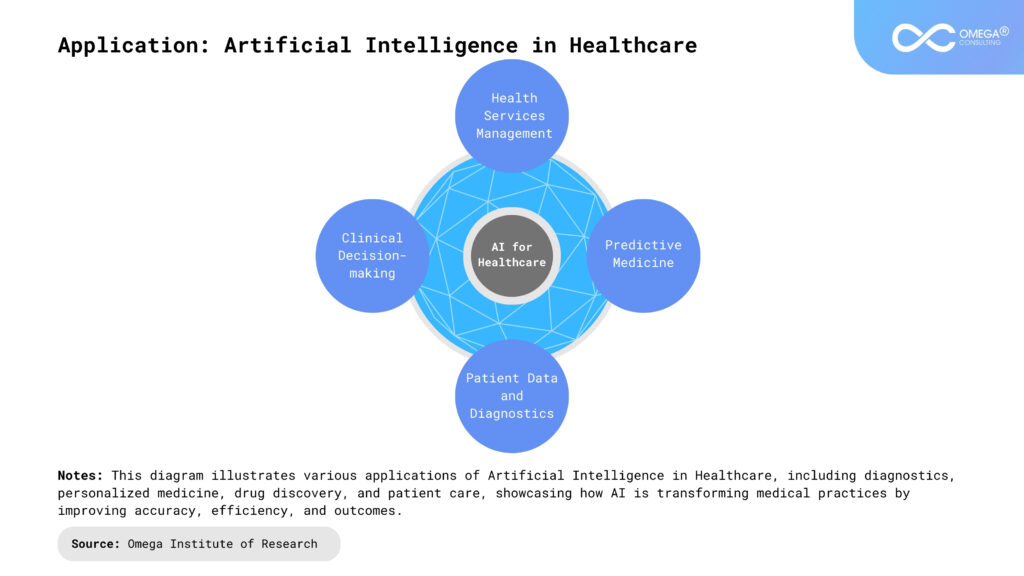
While AI’s functions run the gamut depending on the field, two main focuses in health care are alleviating administrative burdens and improving access.
The administrative burden of health care is immense, and it contributes to provider burnout. In some places, AI is helping by pre-populating providers’ written communications with patients. The provider still reviews the message, makes any necessary adjustments, and manually sends it to the patient, but the AI-created draft may save the provider both cognitive burden and time.
Other places are using AI as an automated medical scribe. Medical scribes are non-clinical staff who take notes during a visit so that the provider can focus on the patient. But could a machine do the same thing? An “ambient scribe” is AI technology that transcribes the conversation during a patient’s visit in real-time. This then becomes the first draft of the provider’s clinic note later.
To improve access to care, AI is being used to fill new needs, like confidential sexual health care. It’s also expanding access to care already provided by human clinicians. For example, a Boston startup is studying if AI can automate a routine dental visit.
But AI can’t do everything, and it faces significant challenges doing the things it can.
Limitation #1 – Data
Data is perhaps the biggest limitation AI faces in health care.
Access to high-quality data is crucial for successful AI implementation. But health care is often fragmented across different systems, leading also to fragmented data. What’s more, experts predict that the amount of health care data in the world will only continue to grow, and faster than other sectors. AI algorithms need to learn how to handle both the quantity of data and a diversity of sources.
With what data are available, a significant concern is bias. While AI-based diagnostic algorithms can certainly help counter providers’ personal biases, they are also susceptible to those same biases. After all, humans are the ones developing the algorithms and inputting the data on which they’re trained.
For example, a 2019 study found that an AI algorithm was under calculating the health care needs of Black patients. A tool used predict sepsis in kids was delaying care for Hispanic patients and algorithms trained on medical imaging can have trouble diagnosing Black or darker-skinned patients.
All told, the quantity and quality of the data available to health care AI technologies – and the management of that data – is key to their success.
Limitation #2 – Costs
Another limitation AI faces in health care is cost. Worth noting, AI may be cost saving in the long run because it cuts down on diagnostic time and other expenses. One estimate suggests that the American health care system could save hundreds of billions of dollars by using AI, and using it well.
But integrating AI solutions into health care workflows requires significant upfront investment. For one, new technology is just expensive. One study found that implementing a new electronic health record in a private practice with just five providers would cost about $162,000 in the first year alone, or over $32,000 per person. For an entire hospital, that number would balloon into the millions.
Purchasing AI isn’t the same as an electronic health record overhaul, but no one should expect it to be cheap. The cost of AI implementation will vary widely based on the type and complexity of the tool purchased: A health system or doctor’s office should expect to spend a couple thousand dollars up to hundreds of thousands of dollars.
Then there are the hidden costs of staff training. We mentioned earlier in the article that the administrative burden on providers is significant. Part of that stress can be from learning new technologies and systems.
That translates to AI, too. There is a risk that forcing staff to learn new systems will lead to job dissatisfaction. If that leads to burnout and that then leads to quitting, the health care system now faces the high costs of turnover.
Limitation #3 – Knowledge Gaps
Lastly, though related to buy-in, AI requires providers to learn new things. Thorough adoption within the health care system will require addressing skill gaps.
There are technical skill deficiencies. Providers may not automatically know how to effectively use AI software or how to seamlessly integrate it with current electronic health records and other operational systems. There are also knowledge gaps in how to apply AI-generated information. Providers may not possess the requisite experience to evaluate the accuracy, reliability, and safety of AI tools. Consequently, they will need to learn how to effectively incorporate AI into their established diagnostic and treatment workflows.
Takeaway
The bottom line is that AI is the future, warts and all. While AI shows great promise for minimizing the administrative burden of health care and improving access, it also comes with significant challenges. Health care systems, providers, and patients will all need to decide which tradeoffs are worth it.
Conclusion
In conclusion, while artificial intelligence presents a transformative opportunity for the healthcare industry, its integration is not without challenges. AI can significantly alleviate the administrative burdens that contribute to provider burnout and enhance access to care. However, issues like fragmented data, high costs, and the need for upskilling pose substantial obstacles. The future of AI in healthcare will depend on how well systems can navigate these hurdles, ensuring that its adoption is both effective and equitable. As AI evolves, the healthcare ecosystem must weigh its benefits against its limitations to ensure that its implementation genuinely enhances care delivery without compromising patient outcomes or provider satisfaction.
Subscribe
Select topics and stay current with our latest insights
- Functions